Certain kinds of food can wear away your teeth. The longer food items adhere to the surface of the teeth, the more acidic and sour your mouth becomes, which can lead to cavities. As this happens, tooth decay begins to form, causing damage to the enamel as it progresses through five phases.
If not treated, tooth decay can damage your gums and teeth until a root canal procedure or tooth extraction is the only solution. Learn about the causes of tooth decay, the process it takes to develop, and how it can be managed.
WHAT IS TOOTH DECAY (CAVITIES / CARIES)?
Dental decay, also known as caries or dental cavities, is a structural issue that occurs when bacteria create acid that causes the tooth to soften and break down.
SYMPTOMS:
The symptoms of tooth decay may differ based on the extent of damage. According to the National Institute of Dental and Craniofacial Research (NIDCR), some people who begin to show tooth decay might have no signs. But as tooth decay progresses, the patient may experience the following symptoms:
- Tooth Sensitivity
- Persistent Tooth Discomfort
- Black or White Areas on Your Teeth
- Bad Breath
- Loose Fillings
- Dental Cavities
- Food Particles Trapped In The Teeth
- Difficulty Consuming Certain Foods
- Abscesses on Teeth Causing Facial Swelling, Pain, and Fever
CAUSES:
A report in the Journal of the American Dental Association (JADA) states that tooth decay can occur due to plaque buildup on the teeth. Plaque is an irritant layer of bacteria that develops on teeth. If you eat sweet or starchy foods, the bacteria within plaque produce acids that damage tooth enamel. Over time, the acids dissolve minerals from the teeth and erode the enamel, leading to tooth decay. Tooth decay can affect anyone at any age.
Someone may be more likely to develop tooth decay if:
- You Have a Dry Mouth
- You Suffer From Weak Enamel Due to Genetics or an Illness
- You Don’t Brush Your Teeth More Than Twice a Day Using Fluoride Toothpaste
- You Suffer From Eating Disorders Like Anorexia or Bulimia
- You Suffer From Gastroesophageal Reflux, Sometimes Referred to as Acid Reflux or GERD
THE STAGES OF TOOTH DECAY:
Plaque is a colorless, sticky film that covers the surface of teeth and is essential in tooth decay. It’s composed of food particles, bacteria, and saliva. If teeth aren’t kept clean, plaque may start to accumulate and become problematic over time, creating tartar. Tartar is believed to harbor bacteria and make them harder to remove. Generally, you can identify five different stages of tooth decay. Let’s examine these stages more closely.
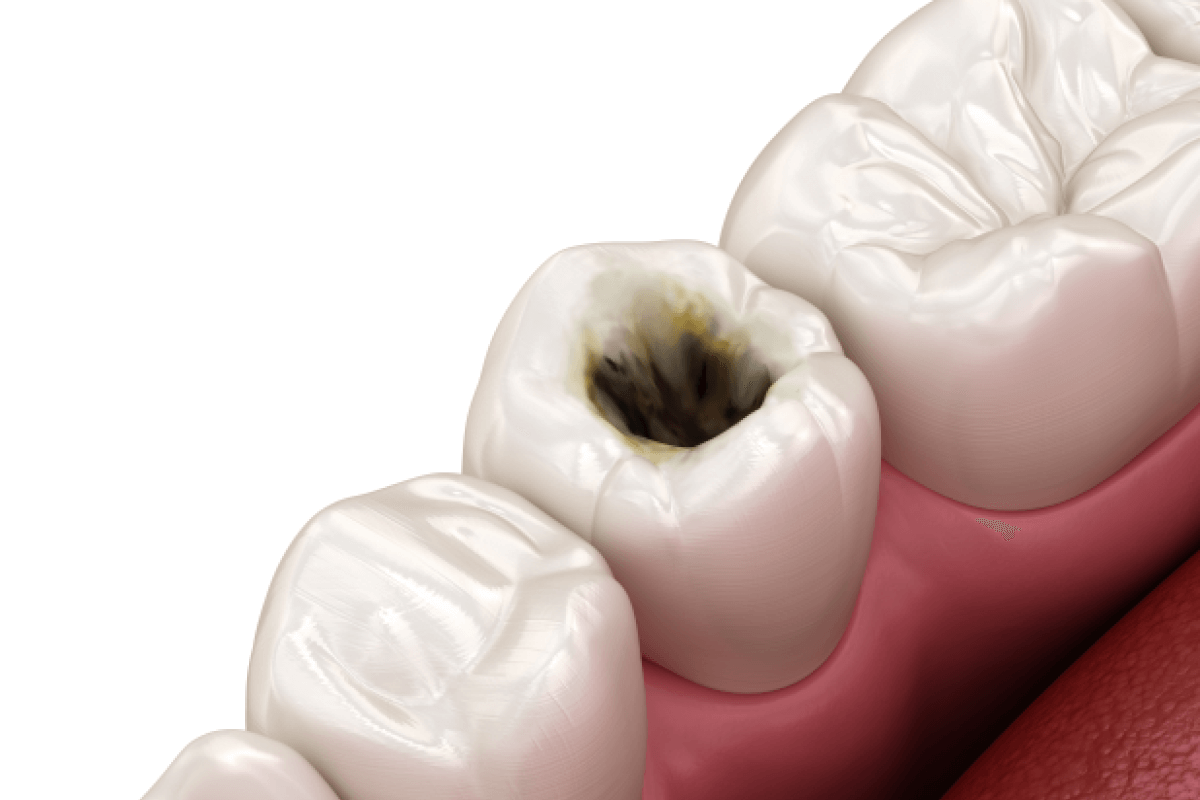
STAGE 1: INITIAL DEMINERALIZATION
The exterior layer of your teeth comprises a type of tissue known as enamel. The enamel is the strongest tissue in your body, largely consisting of minerals.
However, when the tooth is exposed to the acids produced by bacteria that cause plaque, the enamel loses minerals. You might notice a small white spot on your teeth. This loss of minerals is the first indication of tooth decay.
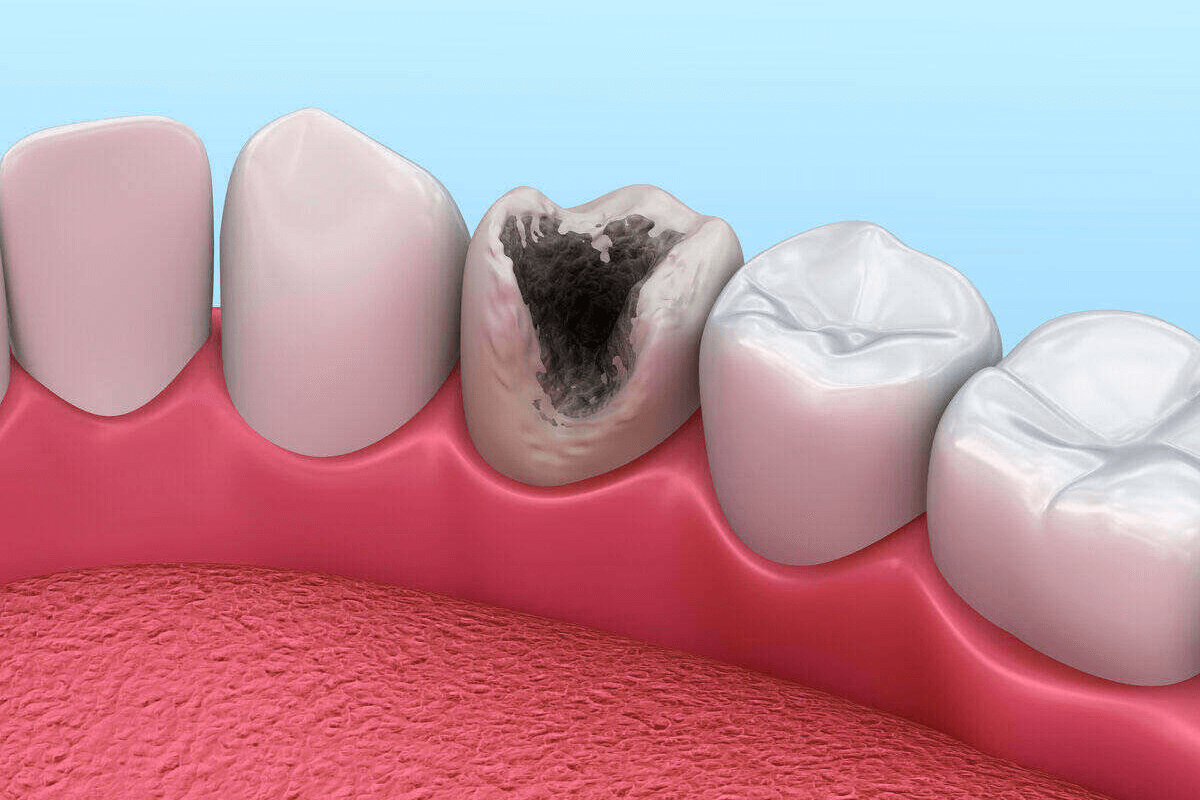
STAGE 2: ENAMEL DECAY
If tooth decay continues, the enamel will break down further. A white spot on the teeth may darken into a brownish shade. As the enamel weakens, tiny gaps in the teeth, known as cavities or dental caries, can develop. Your dentist will need to fill these cavities.
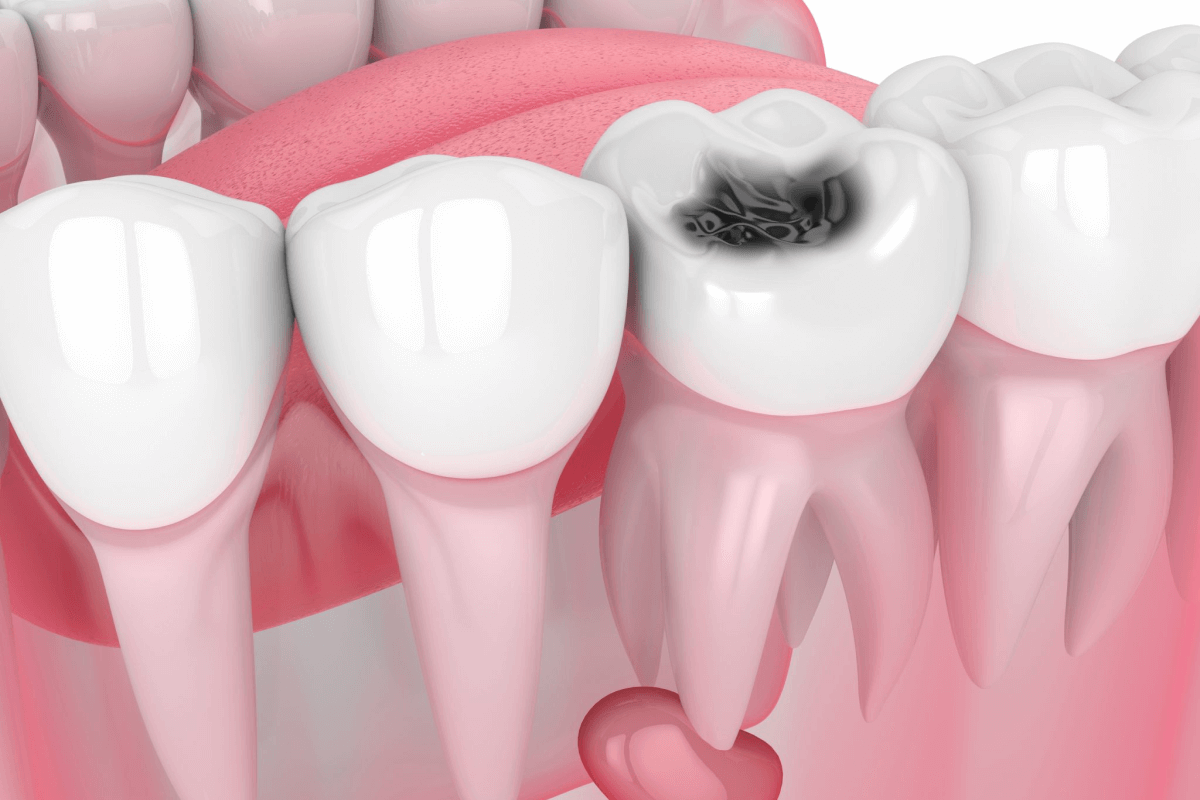
STAGE 3: DENTIN DECAY
Dentin is the layer of tissue beneath the enamel. It’s more brittle than enamel, making it more susceptible to acid. When tooth decay reaches the dentin, it tends to worsen faster, as the dentin includes tubes that are connected to the teeth’s nerves.
If dentin is damaged by tooth decay, you might experience sensitivity, especially to hot or cold drinks or food items.
STAGE 4: PULP DAMAGE
The pulp is the deepest layer within the tooth. It contains nerves and blood vessels that help keep the teeth healthy, and the nerves in the pulp provide sensation. If the pulp is damaged, it can become inflamed and start to swell. Since the tissues surrounding the tooth don’t expand to accommodate the swelling, pressure can be put on nerves, causing pain.
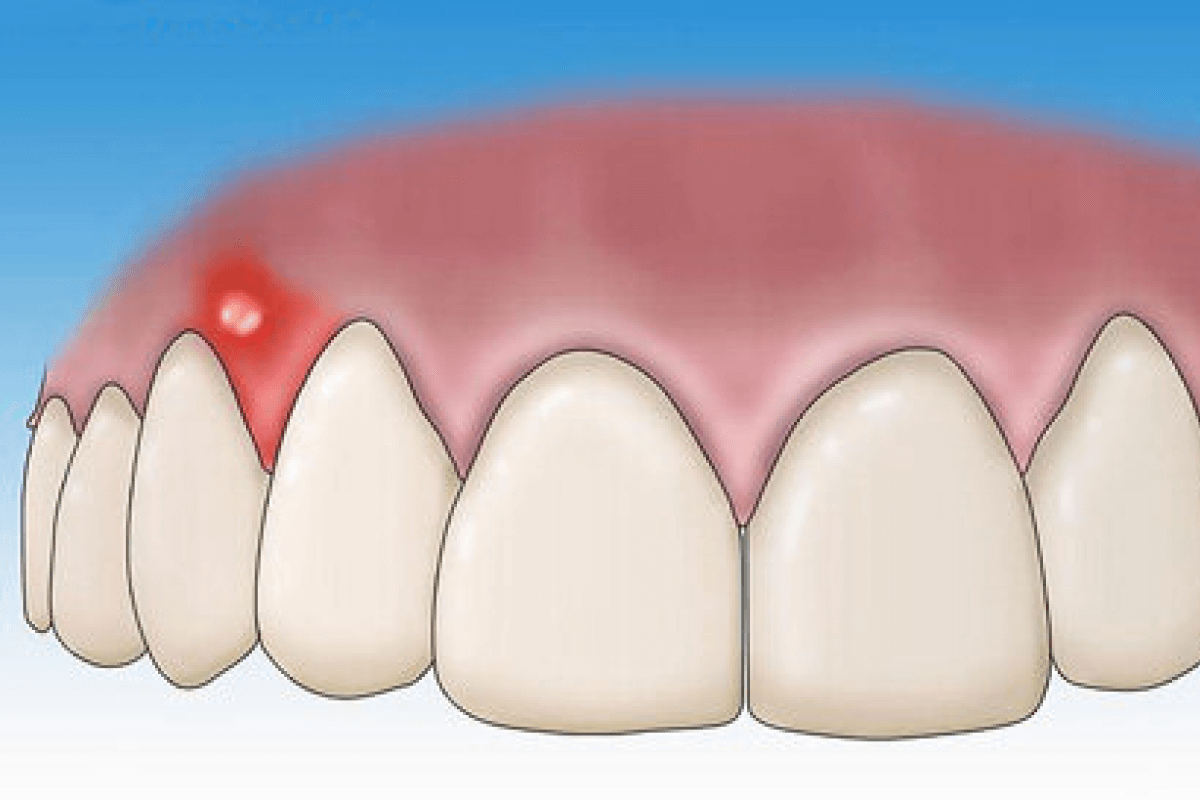
STAGE 5: ABSCESS
When tooth decay reaches the pulp, bacteria may invade and result in an infection. Increased inflammation can lead to a pus-filled pocket at the root of the tooth, known as an abscess. Abscesses in the mouth can cause extreme pain, which may radiate to the jaw. Other signs can include gum swelling, face or jaw swelling, fever, and swelling of lymph nodes in your neck.
An abscess requires urgent treatment since the infection may spread to the jaw bones and other parts of the neck and head. In specific cases, extracting the problematic tooth may be part of the treatment.
TREATMENT:
Frequent dental checkups can spot problems and cavities early, helping to avoid more significant issues. The sooner you get treatment for dental problems, the better chance you have of reversing the initial stage of tooth decay and preventing it from worsening. If you treat a cavity before it causes pain, you likely won’t require extensive treatment.
Treatment for cavities depends on the severity of the problem and the circumstances. Options include:
FLUORIDE TREATMENTS:
If you have a cavity that has just begun, fluoride treatment can strengthen your tooth’s enamel and, in some cases, reverse a cavity at the early stages. Professional fluoride treatments are more concentrated than toothpaste, tap water, or mouth rinses. They can be gel, liquid, foam, or varnish applied to your teeth or placed in a small tray on your teeth.
FILLINGS:
Also known as restorations, fillings are the primary treatment for cavities. Fillings are made from various materials, including dental composite resin and dental amalgam, a blend of multiple substances.
CROWN:
If you have significant decay or weak teeth, you might need a crown, an individually fitted cover that replaces the tooth’s natural crown. The crown protects the tooth’s integrity, reducing the likelihood of breaking. The dentist will remove the decayed portion and enough of the remaining tooth to ensure a proper fit. Crowns can be made of gold, high-strength porcelain, resin, or porcelain bonded to metal or other materials.
ROOT CANALS:
If decay has reached the inner tissue of your tooth, known as the pulp, a root canal may be necessary. This procedure fixes and saves a severely affected or damaged tooth instead of removing it. The damaged tooth pulp is removed, and sometimes medicine is inserted into the canal to eliminate any infection. The pulp is then replaced with a filling.
TOOTH EXTRACTIONS:
Some teeth are so severely damaged that they cannot be repaired and must be extracted. Removing a tooth may leave a gap that allows your other teeth to shift. If possible, consider getting an implant, bridge, or dental implant to fill the missing tooth.
THE BOTTOM LINE:
Dental decay affects your teeth due to bacteria residing in plaque. These bacteria convert sugars in your diet into acids, which harm your teeth. There are five stages of tooth decay. The first stage is usually reversible, while later stages may cause permanent harm to the affected tooth. Treatment options vary depending on the stage. Possible treatments include fluoride treatments, fillings, and root canals. You can take steps to keep your teeth healthy and free of decay by brushing at least once daily, avoiding sweet foods, and seeing your dentist regularly.